Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
4 Minutes
Jorge Gonzalez-Martinez, MD, PhD
One of the main goals of epilepsy surgery is the complete resection (or complete disconnection) of the cortical areas responsible for the primary organization of the epileptogenic activity. This area is also known as the epileptogenic zone (EZ). As the EZ can eventually overlap with functional cortical areas (eloquent cortex), preservations of these necessary brain functions is another goal of any surgical resection in patients with medically refractory epilepsy.
 As successful resective epilepsy surgery relies on accurate preoperative localization of the EZ, a pre-surgical evaluation is necessary to obtain the widest and most accurate spectrum of information from clinical, anatomical, and neurophysiological aspects, with the ultimate goal of performing an individualized resection for each patient. The non-invasive methods of seizure localization and lateralization (scalp EEG, imaging, MEG, etc.) are complementary and results are interpreted in conjunction, in the attempt to compose a localization hypothesis of the anatomical location of the EZ.
As successful resective epilepsy surgery relies on accurate preoperative localization of the EZ, a pre-surgical evaluation is necessary to obtain the widest and most accurate spectrum of information from clinical, anatomical, and neurophysiological aspects, with the ultimate goal of performing an individualized resection for each patient. The non-invasive methods of seizure localization and lateralization (scalp EEG, imaging, MEG, etc.) are complementary and results are interpreted in conjunction, in the attempt to compose a localization hypothesis of the anatomical location of the EZ.
When the non-invasive data is insufficient to define the EZ, extra-operative invasive monitoring may be indicated. Stereo electroencephalography (SEEG) is one of the extra-operative invasive methods that can be applied in patients with medically refractory focal epilepsy in order to anatomically define the EZ and the possibly related functional cortical areas.
The SEEG method was originally developed by Jean Talairach and Jean Bancaud during the 1950s and was mostly used in France and later in Italy, as the method of choice for invasive mapping in refractory focal epilepsy.
In France, after the development of the stereotactic techniques and frames, which were applied initially for abnormal movement disorder surgery, Talairach devoted most of his activity to the field of epilepsy. Bancaud joined Talairach in 1952 and the new methodology created by both physicians led them to depart very quickly from the current approaches. Wilder Penfield and colleagues at the Montreal Neurological Institute did likewise.
Talairach’s ultimate goal was to implement a working methodology for a comprehensive analysis of morphological and functional cerebral space. His atlas on the telencephalon, published in 1967, perfectly illustrates the new anatomical concepts for stereotaxis.
The development of tools, adapted to a new stereotactic frame designed by Talairach and colleagues, allowed Talairach and Bancaud to propose the functional exploration of the brain by depth electrodes, allowing the exploration of both superficial and deep cortical areas. The debut of SEEG was in 1957, when the first implantation of intracerebral electrodes for epilepsy was performed on May 3 at Saint Anne Hospital in Paris, France. By departing from the then current methods of invasive monitoring, such implantations allowed for the exploration of the activity of different brain structures and for the recording of the patients’ spontaneous seizures. This was something that Penfield’s method of investigation failed to achieve. In 1962, Talairach and Bancaud named the new technique and method “the Stereo-Electro-Encephalography.”
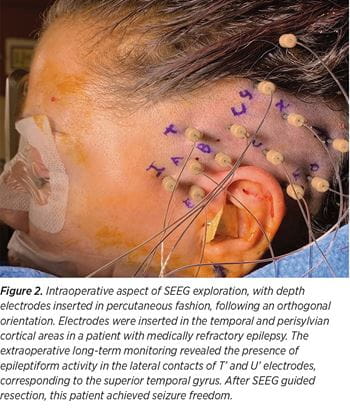 The principles of SEEG methodology remain similar to the principles originally described by Talairach and Bancaud, which are based on anatomo-electro-clinical correlations (AEC) with the main aim to conceptualize the three-dimensional spatial-temporal organization of the epileptic discharge within the brain. The implantation strategy is individualized, with electrode placement based on pre-implantation hypotheses that takes into consideration patient’s seizures’ electro-clinical correlations and their relation with a suspected lesion. The SEEG implantations are performed under robotic guidance, guided by precise pre-implantation hypothesis of localization (See Figure 1). The pre-implantation AEC hypotheses formulation is the single most important element in the process of planning the placement of SEEG electrodes (See Figure 2). If the pre-implantation hypotheses are incorrect, the placement of the depth electrodes will be inadequate and the interpretation of the SEEG recordings will not give access to the definition of the epileptogenic zone.
The principles of SEEG methodology remain similar to the principles originally described by Talairach and Bancaud, which are based on anatomo-electro-clinical correlations (AEC) with the main aim to conceptualize the three-dimensional spatial-temporal organization of the epileptic discharge within the brain. The implantation strategy is individualized, with electrode placement based on pre-implantation hypotheses that takes into consideration patient’s seizures’ electro-clinical correlations and their relation with a suspected lesion. The SEEG implantations are performed under robotic guidance, guided by precise pre-implantation hypothesis of localization (See Figure 1). The pre-implantation AEC hypotheses formulation is the single most important element in the process of planning the placement of SEEG electrodes (See Figure 2). If the pre-implantation hypotheses are incorrect, the placement of the depth electrodes will be inadequate and the interpretation of the SEEG recordings will not give access to the definition of the epileptogenic zone.