Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
3 Minutes
Raymond F. Sekula Jr., MD, MBA
A man begins supper with his wife and takes a bite of bread. He immediately notes a feeling of “electricity” spreading throughout one side of his face. Almost as soon as the pain has struck, it has vanished. He remembers a similar feeling in his hand and arm while playing with an electrical outlet as a child. In that instance, however, his mother explained the cause and how to avoid a similar experience. Although he does not know it, this episode of facial pain represents the beginning of a journey that may or may not end well.
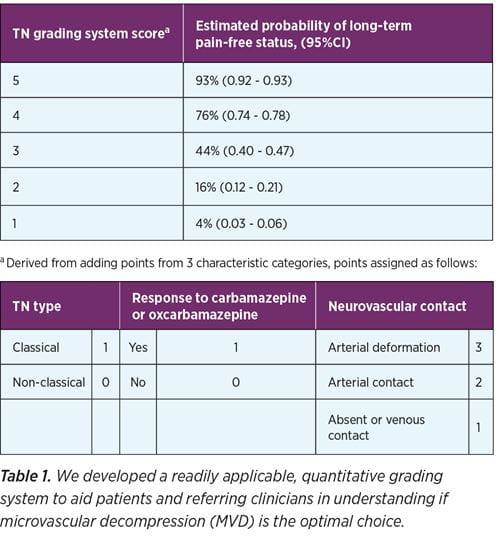
In the Center for Brainstem and Cranial Nerve Disorders, we are working to better understand which patients with trigeminal neuralgia (TN) can benefit from surgical intervention. We know that patients with classical trigeminal neuralgia (cTN) fare better than those with other types of TN. Information gleaned from a detailed history (i.e., a short conversation between patient and physician) allows the physician to make a diagnosis of cTN. Patients with cTN describe sharp, intermittent facial pain usually lasting for a few seconds or less and never longer than a minute or so. This pain does not encompass the posterior third of the scalp or the ear.
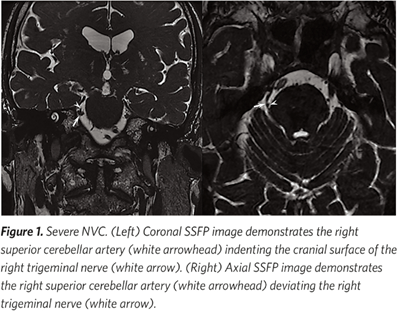 Triggers include innocuous stimuli such as light touch, wind, or chewing. Attacks may occur numerous times each day with periods (i.e., days to months) of remission. Sensory deficit (i.e., orofacial numbness) is not a related symptom. Most patients with cTN will wince (i.e., the so-called “tic doloreux” or painful spasm) with pain. All patients with cTN will benefit from a neurosurgical consultation. Approximately 85% of patients with cTN will have evidence of vascular compression of the trigeminal nerve by high-resolution MRI T2 images. In our Center, we perform high-resolution imaging (Figure 1) on a higher MRI magnet (i.e., 3T) than found in community hospital MRI machines. Those patients with cTN without evidence of neurovascular conflict or an inability to tolerate a general anesthetic are referred for ablative procedures to the trigeminal nerve.
Triggers include innocuous stimuli such as light touch, wind, or chewing. Attacks may occur numerous times each day with periods (i.e., days to months) of remission. Sensory deficit (i.e., orofacial numbness) is not a related symptom. Most patients with cTN will wince (i.e., the so-called “tic doloreux” or painful spasm) with pain. All patients with cTN will benefit from a neurosurgical consultation. Approximately 85% of patients with cTN will have evidence of vascular compression of the trigeminal nerve by high-resolution MRI T2 images. In our Center, we perform high-resolution imaging (Figure 1) on a higher MRI magnet (i.e., 3T) than found in community hospital MRI machines. Those patients with cTN without evidence of neurovascular conflict or an inability to tolerate a general anesthetic are referred for ablative procedures to the trigeminal nerve.
A patient’s response to the antiseizure drug carbamazepine or oxcarbamazepine provides helpful information for the clinician. Many patients report rapid relief of facial pain within just minutes of the first tablet or two of these drugs. While we do not fully understand why response to the drugs is an important predictor of response to neurosurgical intervention, we do know that it is important.
Komal Eubanks, DNP, CRNP, also contributed to this article.