Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
3 Minutes
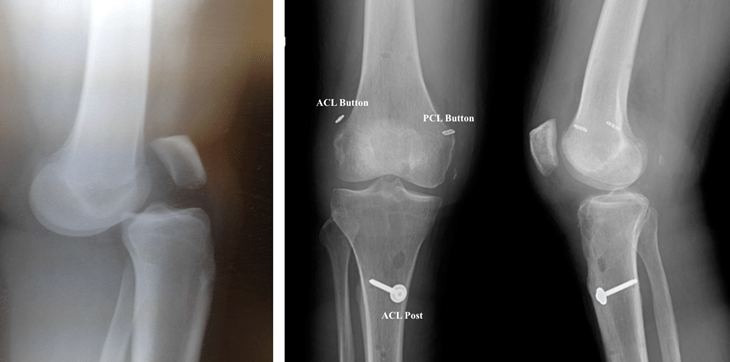
A multi-ligament knee injury (MLKI) occurs when two or more ligaments of the knee are injured, which can include the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), or lateral collateral ligament (LCL). Many factors can affect clinical outcomes and complications after a complex MLKI. But certain aspects of the treatment algorithm for MLKI, such as the timing of surgery, remain controversial.
Researchers and orthopaedic surgeons from the UPMC Department of Orthopaedic Surgery, in collaboration with colleagues from other health systems (recognized below), developed a case-control study to determine the risk factors for common complications after MLKI reconstruction. James Irrgang, PhD, Volker Musahl, MD, Bryson Lesniak, MD, Ravi Vaswani, MD, and Neel Patel, MD, round out the University of Pittsburgh team.
The team conducted a retrospective review of 134 patients with MLKI who underwent reconstruction between 2011 and 2018 at a single academic center. Patients included in the review had a planned surgical reconstruction of >1 ligament based on clinical examination and magnetic resonance imaging (MRI). Complications were categorized as follows:
The potential risk factors for complications included:
Significant risk factors for complications were analyzed by t test, chi-square test, and Fisher exact test.
A total of 108 patients met the inclusion criteria; of these, 29.6% experienced at least one complication. Smoking (odds ratio [OR], 3.20 [95% CI, 1.28-8.02]; P = .01) and planned staged surgery (OR, 2.71 [95% CI, 1.04-7.04]; P = .04) significantly increased the overall risk of complication, while increased time from injury to surgery (OR, 0.99 [95% CI, 0.98-0.998]; P < .01) significantly decreased the risk. Increasing time from injury to surgery (OR, 0.99 [95% CI, 0.97-0.998]; P = .02) also led to a slight, but significantly decreased, risk for arthrofibrosis.
Ultimately, the study findings suggest that smoking, decreased time from injury to initial surgery, and planned staged procedures may increase the rate of complications. Further studies are needed to determine which changes in the treatment algorithm are most effective to reduce the complication rate in patients.
Read more here.
Collaborators not affiliated with the University of Pittsburgh:
Jayson Lian, MD
Montefiore Health System
Michael Nickoli, MD
OhioHealth Physician Group