Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
13 Minutes
Robert A. Kaufmann, MD, professor of Orthopaedic Surgery at the University of Pittsburgh School of Medicine and an upper extremity specialist with UPMC Orthopaedics and Sports Medicine, has been developing a surgical approach and implant system over the last 14 years designed to address the rare but disabling clinical challenge of bidirectional elbow instability.
Elbow instability is typically one of two types: unidirectional or bidirectional. Unidirectional cases represent the majority of sports-related injuries, including ulnar collateral ligament (UCL) tears. Established reconstructive techniques for unidirectional instability, including “Tommy John” procedures, have a long history of development, surgical expertise, robust implant designs, and excellent long-term outcomes. However, elbows with bidirectional instability where both the medial (MCL) and lateral (LCL) ligaments are dysfunctional, are much rarer and suboptimally addressed surgically by the existing reconstruction and stabilizing approaches.
“Patients with bidirectional instability frequently have a history of trauma followed by multiple failed surgeries. Once both sides of the elbow have been disrupted, restoring stability becomes exponentially more complex,” says Dr. Kaufmann.
Patients with bidirectionally unstable elbows often present with severe loss of function and may be unable to perform basic activities of daily living, including feeding, dressing, lifting, and driving a car. Once the elbow is unstable it is prone to the development of osteoarthritis.
“Chronically unstable patients cannot be managed with conservative treatment. When the elbow dislocates with basic movement, it affects everything from feeding and dressing to driving and lifting objects,” says Dr. Kaufmann. “In one of my patients’ the elbow was so unstable that the elbow would subluxate with the force of gravity alone.”
Surgical intervention before arthritis develops is important and, yet, frequently the damage to the cartilage is already present by the time the patient presents to the surgeon but the bone anatomy is often mostly preserved. These patients are frequently young and exhibit substantial durability requirements, meaning they do not want to maintain a lifelong lifting restriction. For these patients, joint resurfacing and ligament reconstruction is employed to recreate stability on both sides. This procedure is known as an interposition arthroplasty, but it is not frequently performed, possibly due to an inability to keep the elbow stable after surgery.
“While interposition arthroplasty has long been explored for younger patients with arthritis, its utility has been limited by the inability to maintain postoperative joint stability — particularly when surrounding ligaments are previously compromised,” says Dr. Kaufmann.
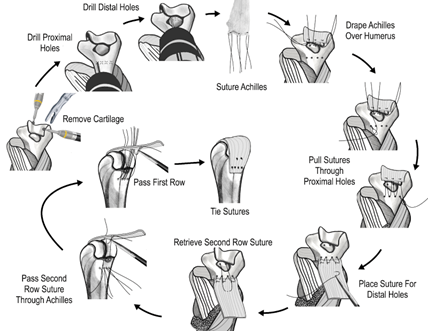
Figure 1. Interposition arthroplasty is performed by resurfacing the distal humerus with an Achilles allograft.
Interposition arthroplasty first removes the arthritic cartilage and then restores a biologic gliding surface by resurfacing the joint with an Achilles tendon allograft over the distal humerus. This process of resurfacing the joint causes instability, which must then be treated through bilateral ligament reconstruction.
Other surgical options for arthritic and unstable joints have included interposition arthroplasty with application of a hinged external fixator or an internal joint stabilizer (IJS), total elbow arthroplasty (TEA) or an elbow fusion. All of these procedures have significant limitations. Hinged fixators have increased risks of infection and require the external fixator to be in place for lengthy time periods. An IJS needs to be surgically removed at a later time. TEA generally means lifelong activity restrictions and has been associated with early loosening in younger patients. Poor salvage options exist once a total elbow fails. Fusions are hard to achieve and sacrifice all motion.
“For younger patients, TEA using cemented implants offers less than ideal long-term outcomes and, for most younger individuals, places unacceptable limits on their activities. For someone already struggling to perform daily tasks, fusion is not a viable option,” says Dr. Kaufmann.

Figure 2. The plates are secured to the proximal ulna with the nuts and bolts as shown in this schematic.

Figure 3. A cylindrical ligament retention device (CLRD) is employed to affix two ligament grafts. It can pass through a hole drilled within the distal humerus and the CLRD maintains equal tension of each graft limb.

Figure 4.Two plates with aggressive teeth are maintained with two bolts and two nuts that secure the tendon grafts against bone.
In order to address this difficult problem, Dr. Kaufmann has designed and developed a novel surgical method and implantable device to restore stability to the elbow. This new bilateral ligament reconstruction system employs a custom-engineered cylindrical ligament retention device (CLRD), which is a machined polyether ether ketone (PEEK) implant that passes through a tunnel in the humerus and is aligned with the elbow’s natural axis of rotation. It serves as a fixed anchor point for ligament grafts on either side of the elbow to recreate the normal architecture. Grafts are trimmed to less than 3.5 mm in diameter and are passed through the tunnel. Placement of these grafts in an isometric location allows for symmetric tensioning of the limbs throughout flexion and extension movements and prevents asymmetric stress from occurring during elbow movement.
The graft limbs are anchored to the ulna through a combination of titanium bolts, nuts and aggressively teethed plates. As the nuts and bolts are tightened, the plates cause substantial compression between the ligament and the bone and lock in the tension that was created by the surgeon within the ligaments, which limits loosening of the reconstruction. This configuration provides equal tensioning of both graft limbs, which has the effect of mimicking native biomechanics and avoids the asymmetry created by separate medial and lateral ligament reconstructions. Additional graft fixation occurs by suturing the native ligaments, capsular remnants, and muscles to the ligament reconstruction limbs.
“Unlike conventional ligament reconstruction, which often relies on two independent grafts tensioned separately and anchored at different points, this approach uses a single device to centralize control of graft tension at the elbow’s natural axis of rotation, avoiding asymmetric loads that can destabilize the joint,” says Dr. Kaufmann.

Figure 5. Biomechanical testing of ligament reconstruction demonstrated no slipping of graft under plate during static and dynamic testing.
Biomechanical testing conducted in Cincinnati and at UPMC supports the reliability of this graft fixation method. Testing with cadaveric elbows subjected to loading from multiple directions at varying positions across multiple flexion angles has shown stability on par with native anatomy. This system also withstood more than 160 N of load, and is stronger than forces the average patient experiences on a daily basis. Thus, this procedure can restore elbow stability in patients for whom conventional procedures have failed or are not viable, particularly younger adults with posttraumatic instability.
“Severe bidirectional elbow instability presents with a limited set of options for patients. Conventional ligament reconstructions are typically unidirectional meaning they reconstruct one side and cannot reliably stabilize both the medial and lateral columns. This approach was designed to restore durable stability to grossly unstable joints,” says Dr. Kaufmann.
Dr. Kaufmann has used his ligament reconstruction under U.S Food and Drug Administration (FDA) compassionate use guidelines in four patients, all with complex, multiply operated upon elbows. Three individuals required their cartilage to be resurfaced. One patient suffered from Ehlers Danlos syndrome (all of her joints are hypermobile and her elbow had dislocated multiple times.) Despite this instability, the cartilage surfaces in this hypermobile patient were intact and she did not need the cartilage to be resurfaced.
We will review one of Dr. Kaufmann’s cases who had undergone multiple failed ligament reconstructions and hardware revisions but still could not bear weight through the limb or maintain elbow alignment. In this case, imaging showed joint subluxation, cartilage loss, and mechanical loosening of the retained implants.
View surgery images down below.
After humeral resurfacing with an Achilles tendon allograft, bilateral tendon grafts were passed through the CLRD and symmetrically tensioned using the aggressively teethed plates. Postoperative alignment was achieved without the need for external fixation, and functional motion was restored.
“These are not high-volume cases, maybe five a year in a state like Pennsylvania, for example. But for the patients who could benefit from this ligament reconstruction, it has the potential to be life-changing. They’ve exhausted everything else, and this approach could offer a chance to regain stability, often for the first time in years,” says Dr. Kaufmann.
Dr. Kaufmann’s implant system is the result of more than 20 years of methodical engineering, surgical iteration, regulatory planning, and collaboration. The ligament reconstruction that is being performed through compassionate use is the initial component of a modular system. The modularity allows ligaments to be reconstructed in isolation, such as has been now done four times through compassionate use. It also allows only the distal humerus to be replaced (hemiarthroplasty) or even both surfaces to be replaced (total elbow arthroplasty). A key feature of both the hemi- and total elbow arthroplasty is the intramedullary screw system that is used for implant fixation. This whole elbow design is now capable of treating a range of elbow conditions based on the patient’s pathology and their anatomic integrity, allowing for patient specific treatment solutions that can be adapted to the patients’ age, durability requirements, and anatomy.
“What we have created is not just a new implant, but a new framework for elbow reconstruction, one that preserves bone stock, restores stability, and can evolve with patient needs over time,” says Dr. Kaufmann.
In 2013, the University of Pittsburgh released the intellectual property, and Dr. Kaufmann founded ARRCH Orthopaedics, LLC, to advance development of this system and FDA engagement. Between 2014 and 2020, the system underwent extensive biomechanical testing and six formal FDA pre-submissions addressing a range of factors, including fatigue strength, graft retention, and wear performance.
“Each presubmission was between 100 and 140 pages. We covered fatigue testing of the bolts and plates and even simulated in vivo joint loading using a cadaveric motion simulator to validate implant and graft behavior under dynamic conditions,” says Dr. Kaufmann.
Dr. Kaufmann then submitted a 510(k) application for the ligament reconstruction portion to establish its substantial equivalence to predicate technology, but after discussions with the FDA regarding the continued concerns related to its novel engineered components, the application was voluntarily withdrawn.
The ligament reconstruction was then used four times through the FDA-approved compassionate use pathway. The FDA was hoping that an Investigational Device Exemption (IDE) study would be initiated that would focus on evaluating the system at multiple sites. Currently under consideration are Duke University, University of Colorado, West Virginia University and The Ohio State University. The IDE will clinically assess how well bidirectional instability can be treated with this bilateral ligament reconstruction system.
“The FDA is supportive of expanding to a multicenter model, which will provide broader clinical validation and facilitate eventual resubmission,” says Dr. Kaufmann.
In addition to the IDE study, Dr. Kaufmann is actively pursuing the development of a cementless hemiarthroplasty (replacement of the distal humerus with a metallic surface) and a total elbow replacement system. Both achieve cementless intramedullary screw fixation of their implanted components and encourage osseointegration. The hemiarthroplasty is intended to serve broader populations, such as those whose distal humerus anatomy is not preserved such as in patients with fracture nonunions or degenerative arthritis not yet requiring full arthroplasty.
“The long term goal is to develop a kit-based solution that allows surgeons to customize reconstruction based on the degree of bone loss and instability. Whether that means resurfacing one side of the joint or both, the ligament reconstruction platform remains foundational,” says Dr. Kaufmann.
Work is ongoing to streamline surgical instruments, reduce component profile, and improve graft passage techniques.

Figure 6. Hemiarthroplasty implantation follows a process of establishing anatomic landmarks and then drilling, cutting and broaching the bone to create a cavity for the implant. A screw is then used to seat the implant while the ligament reconstruction limbs are located at the point of isometry for later attachment to the olecranon.

Figure 7. Total elbow arthroplasty includes the humeral component and the ulnar component both of which achieve intramedullary screw fixation.
“This project wasn’t conceived with commercialization as the end goal. It’s been about helping patients who have no remaining options. Even if we only help a handful of people each year, the effort that has gone into this project will have been repaid many times over as far as I’m concerned,” says Dr. Kaufmann.
Below is a selection of research published by Dr. Kaufmann and colleagues on their novel approach for treating bidirectionally unstable elbow joints.
Dr. Kaufmann owns Arrch Orthopaedics, which has developed this novel method of simultaneous ligament reconstruction.
Robert A. Kaufmann, MD
Professor
UPMC Department of Orthopaedic Surgery

Figure 8. The elbow is dislocated, and the distal humerus has been resurfaced with the Achilles autograft and the ligament reconstruction limbs are being pulled into the distal humerus.
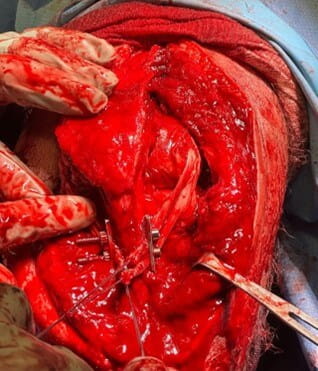
Figure 9. The elbow is reduced, and the grafts have been placed under the aggressively teethed plates and will be tensioned shortly. Once tensioned, the nuts and bolts are tightened to lock in the tension within the graft limbs.