Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
6 Minutes
Ryan McEnany, MD
Assistant Professor of Surgery, UPMC Division of Vascular Surgery
Natalie Sridharan, MD
Fellow, UPMC Division of Vascular Surgery
Aortoiliac occlusive disease can be managed by different surgical and endovascular approaches. In addition to in-line operative reconstruction and extra-anatomic bypass, aortic endarterectomy can provide symptoms relief in selective cases when the aortic pathology is locally confined.This rarely performed surgery in the modern era provides a durable option for AOID in very selective patients.
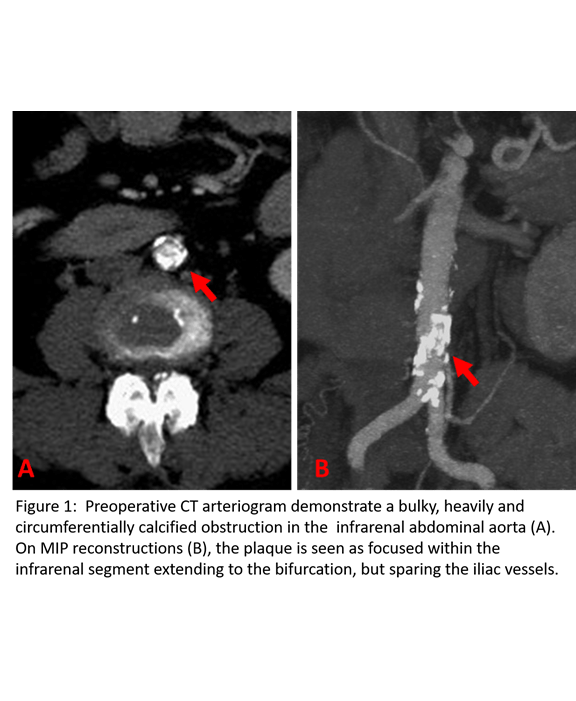
A 61-year-old female presented with a two-month history of right foot pain and discoloration of the first and fifth toe. On questioning, she also noted a history of significant short distance thigh and buttock claudication for the last several months. She was relatively healthy at baseline with a history of hypertension and hyperlipidemia,but a substantial smoking history of two and a half packs per day for 30 years. Her surgical history was notable only for a previous back surgery. On examination, she had reddish discoloration of her right first and fifth toes. She also had no palpable femoral or distal lower extremity pulses. Noninvasive vascular testing revealed flattened pulse volume recording bilaterally from the high thigh to the digit suggesting significant aortoiliac disease. A CTA of the abdomen and pelvis with runoff was obtained which showed a nearly occlusive coral reef-like plaque isolated to the distal aorta just above the bifurcation with some mural thrombus extending proximally close to the level of the renal arteries and essentially normal iliac arteries and distal runoff. (Figure 1) Preoperative testing included a normal stress test.
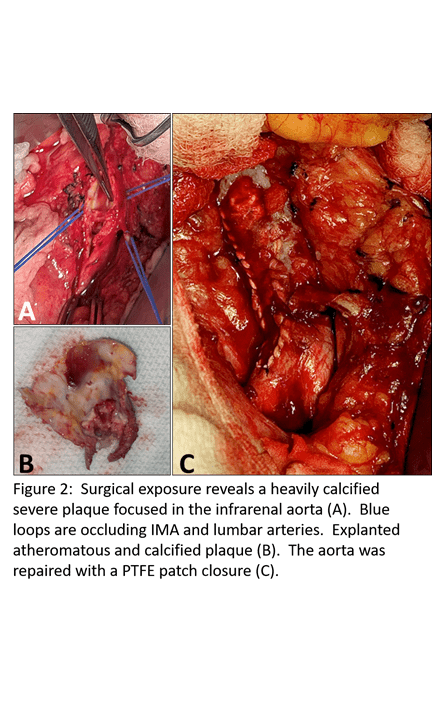
Given her severe claudication symptoms as well as likely embolic events to the toes, the patient was taken to the operating room for aortic endarterectomy via a midline laparotomy. After dissecting the infrarenal aorta and controlling the IMA and all lumbar arteries, clamps were placed on the infrarena aorta and both iliacs, which again, were essentially normal vessels. A longitudinal arteriotomy from just distal to the level of the renal arteries to near the bifurcation revealed a nearly occlusive shelf of plaque in the distal aorta which was endarterectomized (Figure2a,b). The infrarenal aorta was small and we elected to close it with a PTFE patch (Figure2c). Postoperatively, she had palpable femoral and pedal pulses. Her claudication symptoms resolved and she was discharged to home on post-operative day nine.
In the past, aortoiliac endarterectomy (AIE) was a common procedure. In fact, in the 1950s and 60s this was the standard treatment of aortoiliac disease1. However, after the development of prosthetic graft material, aorto-bifemoral (ABF) bypass largely replaced AIE as the treatment of choice for this disease pattern. Today, endovascular treatment, which has shown reasonable long-term patency even incomplex lesions, has largely supplanted the bulk of open treatment of this disease process.
That said, there is a subset of patients with disease confined locally to the distal aorta and common iliac arteries for whom this operation is still appropriate. These patients, as in our case presentation, tend to be younger patients presenting with hip/buttock claudication1. At least half are women and they tend to be heavy smokers1. Pros of this operation include the ability to avoid prosthetic material if desired and the continuity of antegrade inflow to the hypogastric arteries.
The technique for AIE is as described in the case above, with exposure of the infrarenal aorta through a midline laparotomy orretroperitoneal incision and dissection of the aorta along its right side to avoid injury to the IMA. The IMA, middle sacral, and lumbar arteries are controlled to provide a bloodless field for endarterectomy. The external iliacs should be palpated and felt to be relatively disease-free in order to perform AIE. In the case of disease extending into the common iliac arteries, which is more extensive than in our case, the external and internal iliac arteries are controlled and alongitudinal arteriotomy is carried onto the right iliac artery. A separate arteriotomy is made on the left common iliac artery avoiding injury to the autonomic nerveplexus which can result in retrograde ejaculation in men1. Endarterectomy is carried out in the standard fashion being careful to avoid entering the adventitia.
Despite its relative rarity, several publications report excellent long-term durability inappropriately selected patients after AIE. Inahara, et al, reviewed their experience with AIE in 180 patients from 1962-1973. They reported 11-year cumulative patency rates of greater than 85 percent and zero infection2. In a slightly more recent publication, Naylor,et al, reviewed their experience with aorto-iliac endarterectomy in 57 patients over an 11-year time period (1974-1985) in the UK, noting the 24 patients required additional procedures during follow up and 14 of these patients actually required conversion to aorto-bifemoral bypass mostly due to recurrent disease in theexternal iliac artery. This suggests thatpatient selection for this procedure is ofgreat importance, and most patients will not have the disease process or anatomy that is best suited for AIE3. They also noted that ongoing smoking after intervention was associated with significantly worse rates of long term patency3. Patients undergoing AIE should be counseled to quit smoking and provided the appropriate resources to help. Over a similar time frame (1970-1990),Connolly et al reviewed 39 patients undergoing AIE and compared them to 166 patients undergoing ABF in that same time period. They noted 10-year primary patency rates of 89.2 percent for AIE and 78 percent for ABF. Graft infection or aneurysmal formation occurred in five percent of ABF patients and zero percent of AIE patients.20 of the 39 AIEs were in female smokers with small vessels, localized disease, and hyperlipidemia as in our case.
As a final note, in the modern era,endovascular therapy may serve a role in maintaining long term patency after AIE. Denom, et al, reviewed 19 patients after AIE who underwent endovascular treatment of recurrent stenosis after AIE. Four patients with recurrent aortic stenosis and 16 with recurrent iliac stenosis (one with both) were treated with angioplasty with selective stenting with 100 percent technical success and primary patency of 96 percent at one year and 76 percent at three years4.
1. Connolly JE, Price T. Aortoiliac endarterectomy: a lost art? Ann Vasc Surg 2006;20:56-62.
2. Inahara T. Evaluation of endarterectomy for aortoiliac and aortoiliofemoral occlusive disease. Arch Surg 1975;110:1458-64.
3. Naylor AR, Ah-See AK, Engeset J. Aortoiliac endarterectomy: an 11-year review. Br J Surg 1990;77:190-3.
4. Derom A, Vermassen F, Ongena K. PTA and stenting after previous aortoiliac