Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
9 Minutes
The Inflammatory Bowel Disease (IBD) Center at UPMC Children’s Hospital of Pittsburgh provides a range of education and transition efforts for patients and their families that are designed to facilitate the move from pediatric to adult IBD care. One of the newer initiatives created within the IBD Center is a novel program called IBD University. IBD University is an internal “graduation program” for young adult patients that introduces new expectations in self-care and reinforces long-term self-management strategies and goals.
 IBD University was originally developed in early 2024 by IBD Nurse Coordinator Billi Marie Meli, RN, in response to a specific pattern observed in the clinic. Patients ages 18 to 22 were struggling to keep appointments, communicate with the team, and maintain continuity of care. Some were still being scheduled by parents. Others were simply not showing up for routine clinic visits or other appointments. There were also inconsistent transition practices across providers, with some extending pediatric care for IBD patients to age 26, and others ending care at 18 or 22. There was a recognized need for a consistent framework to help young adults assume responsibility for their care.
IBD University was originally developed in early 2024 by IBD Nurse Coordinator Billi Marie Meli, RN, in response to a specific pattern observed in the clinic. Patients ages 18 to 22 were struggling to keep appointments, communicate with the team, and maintain continuity of care. Some were still being scheduled by parents. Others were simply not showing up for routine clinic visits or other appointments. There were also inconsistent transition practices across providers, with some extending pediatric care for IBD patients to age 26, and others ending care at 18 or 22. There was a recognized need for a consistent framework to help young adults assume responsibility for their care.
“Some of our older teens were capable of managing their appointments and medications, but no one had formally asked them to do it yet,” says Meli. “We wanted to standardize expectations and give them a structure that would prepare them for adult care.”
The program’s design accounts for the practical and developmental challenges the team observed with their older patients by combining skill-building, accountability, and graduated responsibility into a framework that emphasizes independence over rigorous supervision.
 “What we were seeing in some of our patients was not a medical issue, but rather a developmental one,” says Whitney Gray, CRNP, pediatric IBD advanced practice provider and leader of the IBD Center’s Transition Program who collaborated in the program’s implementation.
“What we were seeing in some of our patients was not a medical issue, but rather a developmental one,” says Whitney Gray, CRNP, pediatric IBD advanced practice provider and leader of the IBD Center’s Transition Program who collaborated in the program’s implementation.
IBD University is offered to patients beginning at the age of 18 as a required part of the IBD Center’s formal transition program. The process starts with a one-on-one discussion that introduces the goals of the initiative, sets expectations for participation, and reviews the timeline for graduation. Patients are asked to take ownership of appointment scheduling, communications with their provider team, infusion coordination for college, medication refill requests, and symptom reporting.
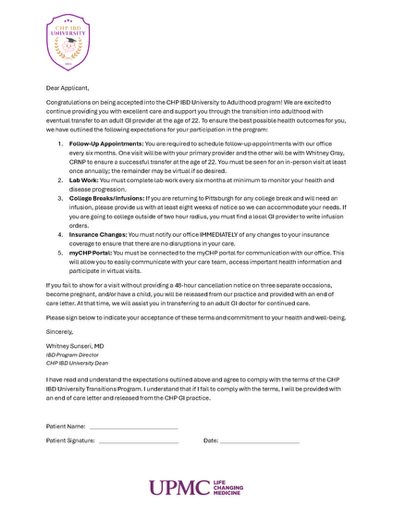 At the center of the program is a written expectation code of conduct, which patients review and sign at the beginning of their IBD University participation. The code of conduct outlines mandatory responsibilities, including showing up for visits, sending messages directly to the care team through the MyCHP digital health portal, and getting regular monitoring lab sand the repercussions of not abiding by the agreement. It also serves as a prompt during follow-up conversations.
At the center of the program is a written expectation code of conduct, which patients review and sign at the beginning of their IBD University participation. The code of conduct outlines mandatory responsibilities, including showing up for visits, sending messages directly to the care team through the MyCHP digital health portal, and getting regular monitoring lab sand the repercussions of not abiding by the agreement. It also serves as a prompt during follow-up conversations.
The document formally referred to as an “acceptance letter”, was drafted by Meli and reviewed by the UPMC Legal Department before implementation. It provides a standardized framework for communication, attendance, and medication management, creating a consistent process across the care team.
“They approved it immediately,” Meli says. “It filled a real gap in consistency and helped us make sure that our patients, parents, and staff were working from a consistent frame of reference with respect to expectations.”
The purpose of the program is to teach accountability through structure rather than to impose penalties. IBD University gives patients the space and tools to practice independence while still being supported by the IBD Center’s clinical team.
“The goal isn’t to punish patients who fall behind or are struggling with something in their lives.” Meli says. “Living with IBD is a difficult thing for everyone to get used, and so is knowing how to care for one’s self. You have teach this like any other kind of skill. IBD University is about showing our patients what engaged participation looks like and helping them build confidence before they move on to adult care.”
The IBD University process is a collaborative effort between the patient and the full multidisciplinary team of the IBD Center. When patients encounter barriers or struggle with certain aspects of their care, the contract serves as a framework for a guided discussion.
“It opens the door to figure out what’s getting in the way,” Meli says. “Sometimes it’s confidence, sometimes it’s logistics, sometimes it’s just learning how to manage adult expectations. Those conversations are an important part of the teaching process.”
Families have responded positively to the structure, particularly the emphasis on graduation. Framing the transition as a milestone rather than a discharge has made the process easier for both patients and parents to embrace.
IBD University begins when patients sign their acceptance letter at age 18 and continues through age 22, aligning with the IBD Center’s broader transition program timeline. Meli and the nursing team track participation, appointment adherence, and engagement throughout this period. The MyCHP digital health portal serves as both a communication tool and a way for patients to demonstrate autonomous behaviors.
“Communication is the biggest piece of this,” Meli says. “They have to be able to call or message us when they need something instead of waiting for their parents to do it.”
Patient progress is documented in the electronic medical record, which includes the signed acceptance letter and ongoing notes indicating the patient’s level of independence. The IBD Center team uses these data to coordinate messaging across providers and to align expectations with families and caregivers.
Meli and the nursing team actively monitor engagement for all participants, tracking missed appointments and adherence as indicators of readiness.
“Our goal is that patients not only follow through with appointments here but also make it to their first adult GI visit,” Meli says. “That’s how we currently define a successful transfer.”
IBD University went live in September 2024. As of December 2025, 186 patients had completed acceptance letters, representing roughly 17 percent of the Center’s 1,100 active IBD population. These structured data help the team identify patients who may need additional outreach before transition.
To evaluate overall readiness for adult care, patients also complete the Transition Readiness Assessment Questionnaire (TRAQ) starting at the age of 12 until their final transition visit with Whitney Gray, CRNP. While not part of IBD University itself, the TRAQ provides complementary insight into each patient’s preparedness for independent disease management as the patient gets older.
IBD University typically takes place over a four year period, but the exact timelines can vary depending on patient readiness and follow-through. Ms. Gray meets with each patient at regular intervals to review progress toward the contract goals and reinforce good behaviors.
The MyCHP digital health portal figures prominently in the process. It serves as a communication tool and a skills platform. “So much in health care comes down to effective communication,” Ms. Gray says. “Not everyone is great at it at first. But it is a skill that can be learned through practice, so we place a great deal of emphasis on understanding one’s condition, history, and needs and how to effectively communicate about it with health care providers.”
Documentation in the patient’s electronic medical record includes the signed IBD University code of conduct, TRAQ scores, and progress notes indicating the patient’s current level of independence. The IBD Center team uses these notes to coordinate messaging across adult providers and to align expectations with the patient’s family or other caregivers.
 After a patient has met all expectations consistently and demonstrated confidence in managing their care, they receive a printed IBD University diploma and are formally documented as a graduate in their medical record. Graduation is often timed to coincide with the final stages of transition planning or the patient’s transfer to adult care.
After a patient has met all expectations consistently and demonstrated confidence in managing their care, they receive a printed IBD University diploma and are formally documented as a graduate in their medical record. Graduation is often timed to coincide with the final stages of transition planning or the patient’s transfer to adult care.
The diploma itself is simple but symbolic. It’s a way to mark a developmental milestone and acknowledge the effort it took to move from dependent care to self-management. For some patients, it is their first formal recognition of this shift.
“Graduation is a chance to say, ‘You’re doing this. You’ve got it,’” Ms. Gray says. “That validation matters a lot to our patients and their families.”
The IBD University initiative has drawn national interest, with abstracts accepted at several conferences in 2025, including Digestive Disease Week (DDW) and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition/Association of Pediatric Gastroenterology and Nutrition Nurses annual meeting. The team’s poster presentation at DDW earlier in 2025, titled “Implementing a Novel Patient-Provider Code of Conduct for Young Adults With Inflammatory Bowel Disease (IBD) to Better Facilitate Transition to the Adult IBD Centers: A Pilot Study,” showcased some early results of the program. In the pilot phase, all 50 patients approached signed the agreement, and no missed appointments were reported in the 60 days following enrollment, suggesting early success in promoting accountability and continuity of care.
The model has also been presented within the Crohn’s and Colitis Foundation’s National Scientific Advisory Council Transition Workgroup and at the UPMC St. Margaret Clinical Research Forum. Collaboration with the adult IBD program at UPMC Presbyterian continues through the annual IBD Unite event, ensuring alignment between pediatric and adult care.
“We’ve had uniformly positive feedback and comments from providers across the country when we present our program’s structure, goals, and success so far,” Ms. Gray says.
Ms. Meli and the IBD Center will continue to refine the structure and metrics of the program. One goal is to better track outcomes longitudinally, including appointment adherence, MyCHP portal usage, and successful transfer to adult care. Another area of work being planned is to develop formal materials that can be shared with other institutions that may want to replicate and adapt the idea to their own program.
“There’s a need for this everywhere,” Ms. Gray says. “We’ve all seen pediatric IBD patients fall through the cracks at this age. If we can catch them before that happens and give them the tools they need, we can likely change the trajectory of their care.”
Learn more about the IBD Center at UPMC Children’s Hospital of Pittsburgh.