Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
8 Minutes
An 18-year-old Caucasian male presented to the UPMC Ear, Nose, and Throat Center with recent onset of painful neck nodules. He denied any swallowing difficulty, hoarseness, or other neck symptoms. He also denied fever, chills, night sweats, or weight loss. There was no history of head and neck radiation exposure.
His past medical history included von Willebrand disease and asthma. His father had passed away from cholangiocarcinoma. There was no family history of thyroid disease, including thyroid cancer. Physical examination showed left sided level III/IV diffuse enlargement of lymph nodes that were nontender and firm to palpation.
Ultrasound imaging of the neck revealed a 1.8 x 1.4 x 1.4 cm heterogenous hypoechoic thyroid nodule and a 2.5 cm left level IV cervical lymph node (see Figure 1). This thyroid nodule met criteria for FNA biopsy according to the American Thyroid Association (ATA) guidelines. Cytology from FNA of the thyroid nodule and lymph node was consistent with medullary thyroid cancer (MTC). Molecular testing with ThyroseqV3 was positive for calcitonin expression and BRAF K601E mutation. Serum calcitonin was significantly elevated at 8268 pg./ml (normal 0-8 pg./ml), supporting the diagnosis of MTC.
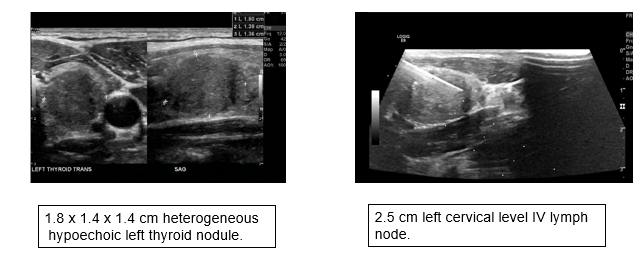
Figure 1: Ultrasound of neck. Left panel showing a 1.8 x 1.4 x 1.4 cm heterogeneous hypoechoic left thyroid nodule. Right panel showing a 2.5 cm left cervical left IV lymph node.
The patient underwent total thyroidectomy with extensive lymph node dissection. Surgical pathology revealed a 2.1 cm primary tumor and 39 out of 41 lymph nodes positive for metastatic MTC with extrathyroidal and extra nodal extension. The margins were uninvolved by carcinoma. C-cell hyperplasia was also noted in background thyroid parenchyma. Pathological stage was pT3N1.
Due to the patient’s young age, presence of an aggressive tumor, C-cell hyperplasia, and unusual molecular findings on cytology aspirate, further testing to evaluate driver mutations and rule out heritable causes was performed. ThyroSeq V3 testing was performed both on the tumor sample and surrounding tissue. BRAF K601E mutation was only noted in the tumor, thus proving that this was a somatic mutation. Interestingly, RET mutation, which is the most common genetic mutation associated with hereditary MTC, was tested negative. The patient did not meet criteria for Familial Medullary Thyroid Cancer (FMTC) or Multiple Endocrine Neoplasia Type 2 (MEN2A).
The patient is continuing his care in the Endocrine Clinic with calcitonin monitoring and serial imaging. Eight months post thyroidectomy he was noted to have an increasing calcitonin level (1,295 pg/mL) and malignant appearing lymphadenopathy on imaging. He underwent selective bilateral neck dissection. Pathology confirmed the presence of metastatic MTC in 13/66 resected lymph nodes. Twenty-two months from initial diagnosis, a doubling of calcitonin (3,622 pg/mL) was observed (see Figure 2). A neck ultrasound at this time showed metastatic appearing lymphadenopathy increasing in size. Due to significant elevation in calcitonin level, and in order to rule out distant metastases, a Ga68-dotatate PET/CT scan was performed. Results did not show distant spread.
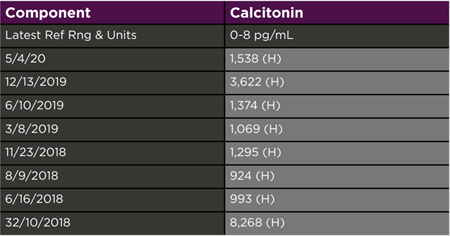
Figure 2: Patient's serum Calcitonin levels over time.
At the patient’s latest follow up visit (27 months after initial diagnosis), the calcitonin spontaneously decreased to 1538 pg/mL. Neck ultrasound showed marginal increase in size of a heterogeneous isoechoic and vascular right supraclavicular level 4/7 nodule when compared to the previous study six months prior. Bilateral nonenlarged and nonspecific cervical lymph nodes were also noted. The impression is that he has persistent but stable locoregional disease. Following extensive discussion with the patient and family, a third surgery was deferred due to high risk of local complications, which possibly include recurrent laryngeal nerve damage, hypoparathyroidism, and low probability of attaining a surgical cure.
Medullary thyroid cancer (MTC) is a neuroendocrine tumor that originates from neural crest derived parafollicular C-cells of thyroid gland, accounting for one to two percent of thyroid cancers in the USA1 (some studies report 3-5% prevalence). MTC can occur sporadically (75%) or can be hereditary (25%)1.
RET proto oncogene (rearranged during transfection) located on chromosome 10q 112 transmembrane receptor of tyrosine kinase family is the most common gene associated with MTC 2. Most patients with MEN2A, 2B and Familial MTC have RET germline mutation and ~ 50% of sporadic MTCs have somatic RET mutation.1,2 Somatic RET codon M918T mutation in sporadic MTC often has an aggressive clinical course.
RET was the first MTC-causing gene to be defined, but several other genes associated with MTC have now also been identified. In one study3, 84 cases of MTC were evaluated with whole-exome sequencing and fluorescence in situ hybridization. The analysis confirmed that mutations in the RET gene are the most common (~50%), followed by mutations in the HRAS and KRAS genes (combined incidence of 20% of MTCs in this study). Furthermore, RAS mutations were only found in sporadic tumors. In addition, a BRAF mutation leading to Lys601Asn (K601N) substitution was identified in one tumor.
BRAF V600E mutations are the most common mutational events in papillary thyroid cancer4,5. BRAF K601E mutations have also been previously described in well-differentiated thyroid cancer but lead to different biological behavior compared to BRAF V600E mutations, causing follicular patterned lesions. The presented case is particularly unique and challenging due to the lack of literature regarding BRAF K601E mutation in MTC. A Greek study6 reported the presence of KRAS [18 of 44 MTC cases- 40.9%] and BRAF V600E [30 of 44 MTC cases- 68.2%], but the MTC related findings have not been replicated in other studies.
In another study3, ALK fusions, including EML4–ALK and GFPT1–ALK, were found in 2% of MTCs [2 out of 98 cases]. EML4– ALK has previously been reported in a variety of cancers but GFPT1–ALK seems to be a novel type of ALK fusion.
With the advent of targeted therapeutics, identification of genetic drivers of cancer has become very important. ALK fusions represent good therapeutic targets and a number of effective ALK inhibitors (such as Crizotinib and Ceritinib) are approved for use in lung cancers that are positive for ALK fusions. One of the patients in this earlier study presented with a metastatic MTC carrying EML4–ALK, which was treated with Crizotinib and showed a clinically significant response. Unfortunately, none of the approved targeted therapeutics for MTC show activity against BRAF. Furthermore, the BRAF V600E targeting drug vemurafenib was not effective in a melanoma patient with BRAF K601 mutation, which potentially limits the targeted therapeutic options for our patient.7
Secretory products of C-cells [Calcitonin and CEA] are valuable tumor markers in MTC8. The serum concentrations of these markers are directly related to C-cell mass. New immunochemiluminometric assays (ICMAs) are highly sensitive and specific for monomeric calcitonin. With ICMAs, cross-reactivity with procalcitonin or other calcitonin-related peptides is largely eliminated, which reduces the need to perform stimulated testing. Calcitonin doubling time of less than six months has been correlated with an adverse prognosis8.
Several imaging modalities are available for ongoing surveillance. Ultrasound examination of the neck is recommended in all patients with MTC1. Contrast-enhanced CT of the neck and chest, three-phase contrast-enhanced multi-detector liver CT or contrast-enhanced MRI of the liver, and axial MRI and bone scintigraphy are recommended in patients with extensive neck disease and signs of regional or distant metastases, and in all patients with a serum Calcitonin > 500 pg/mL1. F-DOPA PET/CT has been shown to have a higher sensitivity in detecting tumor load and extent of disease while FDG-PET/CT is more accurate in identifying disease progression9. Ga68-dotatate PET/CT has been noted to be superior at detecting bone metastatic lesions10. After a prior negative contrast enhanced CT scan of the chest, abdomen, and pelvis in the setting of rapidly rising calcitonin levels, the Ga68-dotatate PET/CT was performed to rule out bone metastases and distant metastatic disease as described above.
This challenging case and literature review are aimed to bring attention to the molecular landscape of MTC and new diagnostic and therapeutic approaches for this frequently aggressive type of thyroid cancer. This case adds information regarding a new genetic mutation associated with MTC.
1. Wells SA Jr, et al, American Thyroid Association Guidelines Task Force on Medullary Thyroid Carcinoma SO Thyroid. 2015;25(6):567.
2. Cerrato A, et al. Molecular genetics of medullary thyroid carcinoma: the quest for novel therapeutic targets. J Mol Endocrinol 43: 143-155. Journal of Molecular Endocrinology. 43. 143-55. 10.1677/JME-09-0024.
3. Ji, J. H. et al. Identification of driving ALK fusion genes and genomic landscape of medullary thyroid cancer. PLoS Genet. 11, e1005467 (2015).
4 Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014).
5. Nikiforova, Marina N et al. “Analytical performance of the ThyroSeq v3 genomic classifier for cancer diagnosis in thyroid nodules.” Cancer, 2018
6. Goutas N, M. BRAF and K-RAS mutation in a Greek papillary and medullary thyroid carcinoma cohort. Anticancer Res. 2008;28(1A):305-308.
7. Moiseyenko FV, et al. Lack of Response to Vemurafenib in Melanoma Carrying BRAF K601E Mutation. Case Rep Oncol. 2019;12(2):339-343. Published 2019 May 16. doi:10.1159/000500481
8. Barbet J, et al. GTE Study Group SO J Clin Endocrinol Metab. 2005;90(11):6077.
9. Ong SC, et al. Diagnostic accuracy of 18F-FDG PET in restaging patients with medullary thyroid carcinoma and elevated calcitonin levels. J Nucl Med. 2007;48(4):501-507. doi:10.2967/jnumed.106.036681
10. Luciana Audi Castroneves, et al. Comparison of 68Ga PET/CT to Other Imaging Studies in Medullary Thyroid Cancer: Superiority in Detecting Bone Metastases, The Journal of Clinical Endocrinology & Metabolism, Volume 103, Issue 9, September 2018, Pages 3250–3259