Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
5 Minutes
Monique C. Chambers, MD, MSL
Fellow, Department of Orthopaedic Surgery
Johnny Huard, PhD
Professor, Department of Orthopaedic Surgery, The University of Texas Health Science Center at Houston
Freddie H. Fu, MD, DSc (Hon), DPs (Hon)
Chairman, Department of Orthopaedic Surgery
Cook Myosite, incorporated in 2002, is an organization that seeks to "reach people affected by muscle-related disorders around the world" through cellular technologies. The company was founded based on experiments conducted at the University of Pittsburgh in the Growth and Development Laboratory, known today as the Stem Cell Research Center. After being recruited to study a potential cure for Duchenne Muscular Dystrophy, Johnny Huard, PhD, isolated a unique cell source that was later termed "muscle-derived stem cells" (MDSC).1,2,3
This translational research story begins in the mid-1990s, and continues today, to investigate the use of MDSCs for musculoskeletal repair. Dr. Huard's initial research was supported through his 2004 AAOS Kappa Delta Young Investigator Award, and his 2018 AAOS Kappa Delta Ann Doner Vaughn Award. Much of the work on muscle-derived stem cell technology did not arise from a deliberate search to find a novel population of muscle cells with high regenerative potential, but was instead conceived in response to setbacks encountered during projects on muscle cell transplantation for Duchenne Muscular Dystrophy (DMD). Failure and negative outcomes in research can serve as valuable learning experiences, and that unexpected results, interpreted with an open mind, can lead to innovative thinking and breakthrough ideas.
DMD is a devastating, inherited X-linked muscular disease characterized by progressive muscle weakness due to a lack of dystrophin expression in muscle fiber sarcolemma. Various approaches to deliver dystrophin to dystrophic muscle have been explored, but no effective treatment exists to alleviate DMD progression. The transplantation of normal myoblasts into dystrophin-deficient muscle created a reservoir of normal myoblasts capable of fusing with each other and dystrophic muscle fibers, restoring dystrophin to the muscle. The myoblast transplantation approach had been hindered by immune rejection and the limited migration and survival of the injected cells.1 In fact, 99 percent of the cells did not survive the implantation. This was seen as a major weakness of the technology. While the vast majority of the scientific community at that time focused on approaches to improve cell survival in the 99 percent of the cells that rapidly died post-implantation, the research team at the University of Pittsburgh, under the chairmanship of Freddie H. Fu, MD, decided to investigate why only one percent of the cells survived post-implantation.
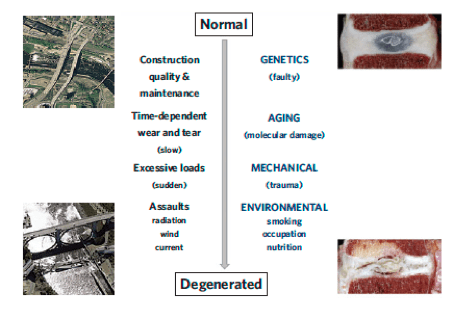
A distinct, slowly adhering cell (SAC) population of myogenic cells were isolated that exhibited a superior ability to regenerate dystrophin-positive muscle fibers.2,3 More importantly, these muscle cells appeared to be a unique population able to survive in the harsh microenvironment of injured tissues after transplantation due to their high expression of antioxidants.4,5 These slowly adhering myogenic progenitor cells were termed muscle-derived stem cells (MDSCs) due to their stem cell-like phenotype and behavior that included increased survival and long-term proliferation, continued self-renewal, and multipotent differentiation ability (Figure 1).
Today, Cook Myosite continues to investigate the utilization of autologous muscle-derived cells (AMDC) in personalized regenerative medicine. Currently, the AMDC technology is being evaluated in clinical trials throughout Canada, Europe, and the United States. This same technology was used by Michael B. Chancellor, MD, to treat patients with stress urinary incontinence (SUI).6,7 The administration of AMDCs in females with SUI is in phase III clinical trials.
On July 31, 2017, Commonwealth of Pennsylvania Governor Tom Wolf toured the company's grounds and celebrated the groundbreaking of its 62,000-square-foot facility expansion to accommodate the demand as they prepare for widespread production. As a result, there has been an increase in the number of jobs provided, with more than 130 employees in the Pittsburgh region.
With a mission to advance the science of personalized regenerative medicine to elevate current therapies to an accepted and accessible option beyond traditional care, we are proud to see the ever-expanding results of more than 20 years of research that began at the University of Pittsburgh. Although this technology has never been used on Dr. Fu's orthopaedic patients, there is great excitement for future research to demonstrate the many ways we can help patients as this technology progresses from the bench to the bedside.
References
1. Day CS, Bosch P, Kasemkijwattana C, Menetrey J, Moreland MS, Fu FH, Ziran B, Huard J. Use of Muscle Cells to Mediate Gene Transfer to the Bone Defect. Tissue Eng. 1999; Apr; 5(2): 119-25.
2. Huard J, Verreault S, Roy R, et al. High Efficiency of Muscle Regeneration After Human Myoblast Clone Transplantation in SCID Mice. J Clin Invest. 1994; 93: 586-599.
3. Qu-Petersen Z, Deasy B, Jankowski R, Ikezawa M, Cummins J, Pruchnic R, Mytinger J, Cao B, Gates C, Wernig A, Huard J. Isolation of a Novel Population of Muscle Stem Cells in Mice: Potential for Muscle Regeneration. J Cell Biol. 2002; 157(5): 851-64.
4. Urish KL, Vella JB, Okada M, et al. Antioxidant Levels Represent a Major Determinant in the Regenerative Capacity of Muscle Stem Cells. Mol Biol Cell. 2009; 20: 509-520.
5. Drowley L, Okada M, Beckman S, et al. Cellular Antioxidant Levels Influence Muscle Stem Cell Therapy. Mol Ther. 2010; 18: 1865-1873.
6. Cannon TW, Lee JY, Somogyi G, Pruchnic R, Smith CP, HuardÊJ, Chancellor MB. Improved Sphincter Contractility After Allogenic Muscle-derived Progenitor Cell Injection Into the Denervated Rat Urethra. Urology. 2003; 62(5): 958-63.
7. Yokoyama T,Yoshimura N, Dhir R, Qu Z, Fraser MO, Kumon H, de Groat WC, Huard J, Chancellor MB. Persistence and Survival of Autologous Muscle Derived Cells Versus Bovine Collagen as Potential Treatment of Stress Urinary Incontinence. J Urol.Ê2001; 165(1): 271-6.