Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
In May, a team of neurosurgeons and otolaryngologists at UPMC performed a first-of-its-kind surgery using a new trans-facial endoscopic approach they developed to treat cases of drug-resistant epilepsy originating in the temporal lobe. The first successful surgery was performed in a woman whose epilepsy originated in areas of the mesial temporal pole, amygdala, hippocampus, and parahippocampus.
The novel surgical approach is called a Sublabial Pittsburgh Endoscopic Temporal Lobe (SPETL) approach. The approach is designed to reach temporal pole and mesial temporal lobe structures for resection via a transfacial or transmaxillary corridor that can avoid injury to healthy functional cortical and subcortical tissues in the temporal lobe that would otherwise be violated by traditional surgical approaches to resections in these areas.
The multidisciplinary team of neurosurgeons who performed the new procedure includes:
Also collaborating on the development of the new approach from the Department of Neurosurgery were visiting fellow Omuvwie Orhorhoro, MBBS, chief resident physician Michael M. McDowell, MD; and assistant professor Georgios Zenonos, MD. Also collaborating was Eric Wang, MD, from the Department of Otolaryngology and UPMC Center for Cranial Base Surgery.
“Even though our newer, minimally invasive surgical approaches and technologies to treat epilepsy have revolutionized the field and led to more precise localization of the epileptogenic zone (EZ) in patients, improved outcomes, and fewer surgical complications, using these techniques and approaches often still requires that we penetrate and disrupt healthy brain tissues to get to the locus of a patient’s seizure generation. This disruption to healthy tissues can have a host of consequences for the patient, such as cognitive disturbances and other deficits," says Dr. Gonzalez-Martinez. "Our new endoscopic approach that transverses the sinus cavity to reach the temporal lobe – where the majority of cases of focal epilepsy originate – is a much more direct path with virtually no disturbance to healthy brain tissues. In addition, there are no visible incisions or the need to remove larger portions of the skull through a craniotomy."
The surgical team began developing the new approach in 2019. Anatomic and procedural studies were conducted in eight cadaveric models prior to performing the first live procedure in May. These studies enabled the surgeons to test and refine the optimal trajectories and corridors through which they could gain access to the temporal lobe and its structures.
"This new approach affords us more direct access to the temporal lobe, allowing the complete treatment of the seizure’s generator areas with minimal disruption of the nonepileptic brain," says Dr. Gonzalez-Martinez.
Since the first successful procedure in May, the surgical team has performed two additional cases using the new SPETL approach. All three patients are currently doing well with an uneventful postoperative recovery to date.
The surgical team is preparing their first manuscript detailing their development of the new approach and findings from its initial use in patients. The surgical team also will look to present their findings at an upcoming meeting of the American Association of Neurological Surgeons.
“We are pioneering a new treatment modality for epilepsy surgery, one that can even further limit or eliminate complications and provide our patients freedom from their seizures," says Dr. Gonzalez-Martinez. "With our combined expertise in epilepsy surgery, endoscopic techniques, and cranial base surgery, I believe that we will expand the use and indications for this approach in well-selected patients through rigorous exploration and experimentation to validate the efficacy and safety of the procedure to achieve optimal outcomes for our patients."
To learn more about the new procedure or discuss a patient case for possible referral, please contact the UPMC Department of Neurological Surgery at 412-647-3685.
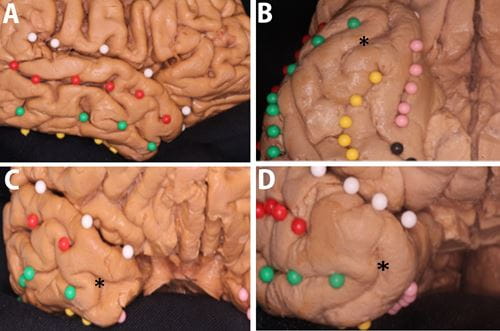
Figure 1
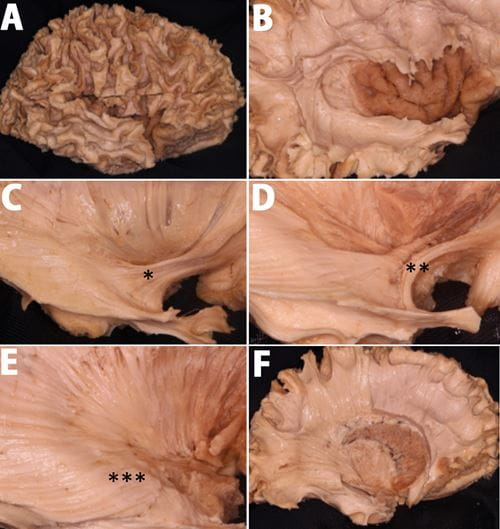
Figure 2
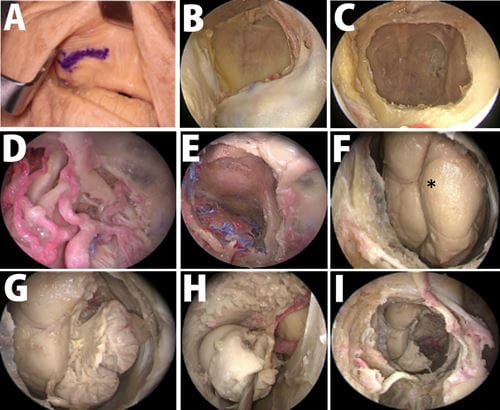
Figure 3
Interested in receiving specialty-specific information? Register for UPMC Physician Resources to get emerging research, clinical updates, and free CME straight to your inbox.