Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
5 Minutes
Esra Karslioglu French, MD
Clinical Associate Professor of Medicine,
Division of Endocrinology and Metabolism
University of Pittsburgh School of Medicine
Linwah Yip, MD, FACS
Co-Chief, Division of Endocrine Surgery
Assistant Professor, Department of Surgery,
Section of Endocrine Surgery
University of Pittsburgh School of Medicine
Graves’ disease (GD) is the most common cause of hyperthyroidism, with an annual incidence of 20 to 50 cases per 100,000 persons.1 Graves’ ophthalmopathy (GO), which can present with proptosis, tearing, and periorbital edema, is detected in up to 50 percent of patients with Graves’ disease. The majority of GO cases are mild, and patients recover after treatment of hyperthyroidism, whereas 5 percent of GD patients will develop moderate to severe GO.
Quality of life (QoL) surveys (i.e., SF-36) show that people with GO have substantially reduced QoL, equivalent to having diabetes or certain cancers.2 Current therapeutic approaches for GO often fail to significantly improve QoL, as patients continue to have changes in their vision and appearance.
When patients are assessed and treated in multidisciplinary thyroid eye clinics, they have a more favorable outcome compared with patients who are not managed in such clinics.3 A survey study of clinicians showed a lack of “best practice” in a significant number of responders for everyday clinical issues, such as urgent referral to an ophthalmologist in case of a possible dysthyroid optic neuropathy.3 The American Thyroid Association (ATA) and European Group on Graves’ Orbitopathy (EUGOGO) recommend the implementation of multidisciplinary thyroid eye clinics for assessment and treatment of GO.4,5
Medical professionals at UPMC have worked together to establish a Multi-disciplinary Thyroid Eye Disease Clinic to improve patient care and satisfaction. This multidisciplinary clinic allows patients to be seen simultaneously by an ophthalmologist and endocrinologist. Endocrine surgery; ear, nose, and throat (ENT); and other specialists are consulted in appropriate cases.
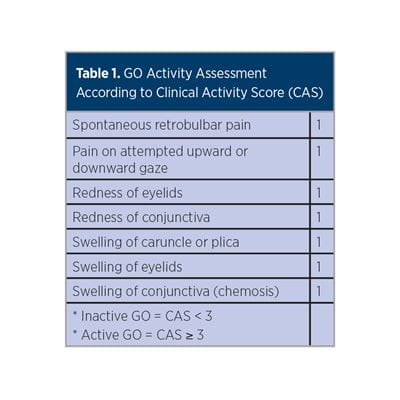
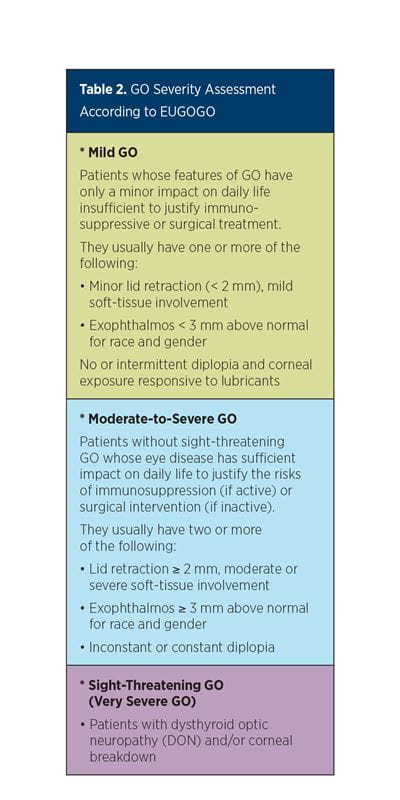
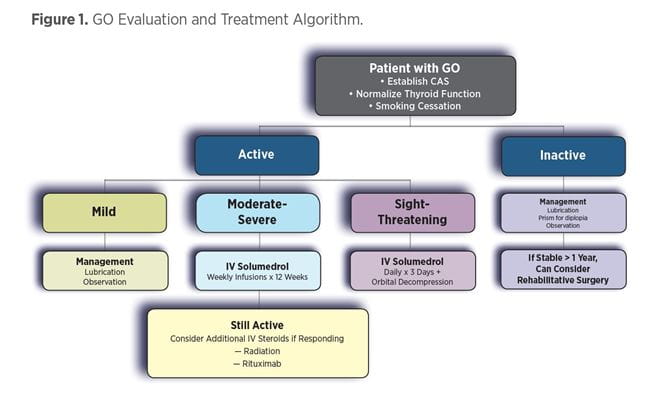
Patients seen in the UPMC Multidisciplinary Thyroid Eye Disease Clinic are first evaluated by using clinical activity score (CAS) (Table 1) and severity (Table 2) assessments to establish the degree of GO while modifiable risk factors are identified. All hyperthyroid patients are treated to achieve euthyroidism expeditiously. Smokers are referred to tobacco cessation centers, as smoking increases the risk for diplopia and proptosis by eight-fold. Selenium, which is shown to improve QoL and overall eye evaluation in patients with GO,6 is recommended. Thyroid-stimulating immunoglobulin (TSI) levels are measured, as TSI predicts GO risk and GO therapeutic response.7
Hyperthyroidism and ophthalmopathy typically occur within one year of each other but can be separated by decades.8 In 10 percent of patients with GO, either thyroid levels remain normal or autoimmune hypothyroidism develops. Radioiodine (RAI) is not recommended in patients with moderate-to-severe or sight-threatening GO, as it can worsen eye disease, possibly due to TSI elevation after treatment. Patients with moderate-to-severe or sight-threatening eye disease are treated by antithyroid drugs (ATD) or thyroid surgery. Thyroidectomy is preferred in patients who have adverse reactions to ATD, enlarged thyroid glands, or a pregnancy in the near future.4
The approach to patients with GO is summarized in Figure 1, which involves local measures, corticosteroids, orbital radiation, and surgery.
GO Challenges Continue
GO continues to be a challenging disease despite the current management options. A recent Phase 3 OPTIC clinical trial showed promising results for the use of the experimental drug teprotumumab, which is a human monoclonal antibody that targets the insulin-like growth factor 1 receptor. When given during the active phase of disease, teprotumumab reversed eyelid swelling, reduced eye bulging and double vision, and improved quality of life.9,10 Teprotumumab is expected to be submitted to the U.S. Food and Drug Administration (FDA) for approval this year.
The Multidisciplinary Thyroid Eye Disease Clinic at UPMC allows patients with GO the opportunity to coordinate multiple visits in a timely manner, which can be a challenging aspect of care for these patients. Comprehensive counseling is provided by experts to aid patients in making appropriate treatment decisions. Our team also aids in educating patients about common misperceptions related to GO.11 The continuing goal of the UPMC Multidisciplinary Thyroid Eye Disease Clinic is to provide multispecialty care to patients with GO and improve outcomes for this challenging disease.
References
1 Smith TJ, Hegedüs L. Graves’ Disease. N Eng J Med. 2016; 375(16): 1552-65.
2 Kahaly GJ, Petrak F, Hardt J, Pitz S, Egle UT. Psychosocial Morbidity of Graves’ Orbitopathy. Clin Endocrinol (Oxf). 2005; 63: 395-402.
3 Perros P, Baldeschi L, Boboridis K, Dickinson AJ, Hullo A, Kahaly GJ, et al. A Questionnaire Survey on the Management of Graves’ Orbitopathy in Europe. Eur J Endocrinol. 2006; 155(2): 207-11.
4 Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016; 26(10): 1343-421.
5 Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, Perros P, Salvi M, Wiersinga WM: The 2016 European Thyroid Association/European Group on Graves’ Orbitopathy Guidelines for the Management of Graves’ Orbitopathy. Eur Thyroid J. 2016; 5: 9-26.
6 Marcocci C, Kahaly GJ, Krassas GE, Bartalena L, Prummel M, Stahl M, et al. Selenium and the Course of Mild Graves’ Orbitopathy. N Eng J Med. 2011; 364(20): 1920-31.
7 Barbesino G, Tomer Y. Clinical Review: Clinical Utility of TSH Receptor Antibodies. J Clin Endocrinol Metab. 2013; 98(6): 2247-55.
8 Bahn RS. Graves’ Ophthalmopathy. N Eng J Med. 2010; 362(8): 726-38.
9 Douglas R. Teprotumumab Treatment Effect on Proptosis in Patients With Active Thyroid Eye Disease: Results From a Phase 3, Randomized, Double-masked Placebo-controlled, Parallel-group, Multicenter Study. Presented at the American Association of Clinical Endocrinologists 28th Annual Scientific and Clinical Congress, April 25-28, 2019,
in San Francisco, California.
10 Smith TJ, Kahaly GJ, Ezra DG, Fleming JC, Dailey RA, Tang RA, et al. Teprotumumab for Thyroid-Associated Ophthalmopathy. N Eng J Med. 2017; 376(18): 1748-61.
11 Edmunds MR, Boelaert K. Knowledge of Thyroid Eye Disease in Graves’ Disease Patients With and Without Orbitopathy. Thyroid. 2019; 29(4): 557-62.