Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
3 Minutes
by David J. Salvetti, MD
Understanding the relationship between chronic opiate usage and surgical outcomes is critical to optimizing patient outcomes while minimizing potentially avoidable complications. Preoperative chronic narcotic usage has been shown to be associated with the inability to wean from narcotics postoperatively, decreased patient-reported outcome scores, and other complications. The purpose of this study was to evaluate the effect of preoperative narcotic use on patient-reported outcomes in the complex adult spinal deformity population.
All patients undergoing complex reconstructive spine surgery performed by the study’s author from 2015 and 2016 were identified. Indications for surgery included iatrogenic flat back deformity, high-grade spondylolisthesis, adult idiopathic scoliosis, severe spondylosis, pseudarthrosis of prior fusion, proximal junctional kyphosis, and hardware failure. Patients with neoplasms, cervical, or cervicothoracic procedures were excluded. The cohort was divided into chronic opiate users and patients who were not chronic users of opiates. Chronic use was defined as evidence in the electronic medical record of opiate use greater than six months prior to surgery with a minimum morphine equivalent dosing of 30mg/day. Statistical analysis was then utilized to determine whether chronic opiate use was negatively associated with health-related quality of life (HRQOL) metrics postoperatively.
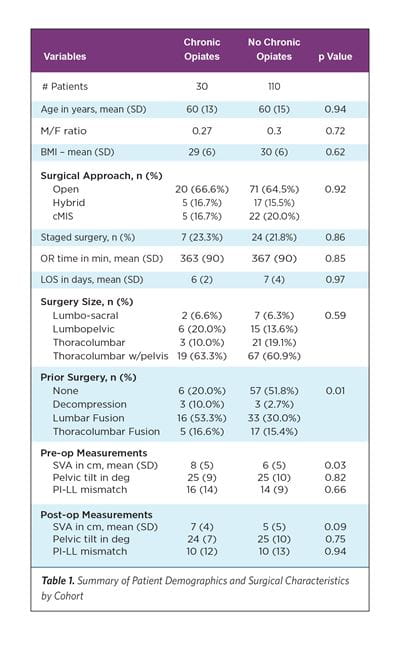
A total of 140 patients were included for analysis. Of these, 30 (21.4%) patients were categorized as chronic opiate users. Baseline pre-op surgical characteristics were analyzed for differences between non-opiate and opiate groups including BMI, age, length of surgery, ratio of males to females, surgical approach, surgical size, length of hospital stay, prior surgery, and spinopelvic measurements.
The opiate group demonstrated slightly worse pre-op sagittal vertical axis (SVA) measurements at a mean of 8 cm versus 6 cm for the non-opiate group (p=0.03). Additionally, 80% of patients in the opiate group had previously undergone spine surgery, versus 48.2% in the non-opiate group (p=0.01). No differences were identified in mean pre-op HRQOL metrics, including the Oswestry Disability Index (ODI), health state, visual analog scale (VAS) for back pain, and EQ-5D indices. At both six weeks and six months post operatively, patients in the opiate group demonstrated worse mean VAS back pain scores relative to the non-opiate group (6wk: 6.25 vs. 4.62, p=.01; There was also no statistical correlation between daily morphine equivalents and ODI scores. Lastly, the change in pre-op to LK follow-up of HRQOL metrics was not statistically different between groups.
In this group of complex spine surgery patients, chronic opiate use was associated with higher patient-reported VAS back pain scores at six weeks and at six months. This is an expected finding given preoperative opiate-induced hyperalgesia. Additionally, chronic opiate use was associated with higher ODI scores at six months and at last known follow-up. Further work is needed to determine whether strategies to wean patients from opiates preoperatively could improve outcomes or whether these differences merely represent a group with more severe pathology.
Note: Kamil Nowicki, MD, PhD; Nitin Agarwal, MD; Nima Alan, MD; Gurpreet Gandoke, MD; D. Kojo Hamilton, MD; Adam S. Kanter, MD; and David O. Okonkwo, MD, PhD, also contributed
to this article.
6mo: 5.4 vs. 4.2, p=.05). At six months postoperatively and at the last known (LK) clinical follow-up, ODI scores were higher in the opiate group (6mo: 42.8 vs. 31.2, p=0.04; LK: 42.4 vs. 31.5, p =0.02). There was no statistical difference in the rate of improvement in any HRQOL metrics between groups.