Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
4 Minutes
Rabih Chaer, MD
Professor of Surgery, UPMC Division of Vascular Surgery
Kathryn Fong, MD
Fellow, UPMC Division of Vascular Surgery
Endovascular aneurysm repair (EVAR) has caused significant change in the algorithm of abdominal aneurysm repair. However, concomitant aneurysms of the common iliac arteries or the iliac bifurcation present challenges to achieving adequate distal seal during EVAR. Traditionally, this has been addressed by either extending the distal seal into the external iliac artery with embolization of the ipsilateral internal iliac artery to prevent type II endoleak, or with ligation and surgical bypass to the internal iliac artery to preserve pelvic perfusion.
Case Report
A 76-year-old male presented to UPMC for evaluation of aortoiliac aneurysm disease. His past medical history is also significant for mild emphysema, hyperlipidemia, lung and prostate cancer, and he has no family history of aneurysmal disease or connective tissue disorder. He is without symptoms of cardiac ischemia or peripheral claudication. His preoperative CT scan demonstrated the presence of a small infrarenal abdominal aortic aneurysm measuring 4.8cm, and bilateral large common iliac artery aneurysms, measuring 4cm and 3.8cm on the right and left, respectively. The internal iliac arteries were patent bilaterally (Figure 1 and 2). He underwent endovascular repair of his abdominal aortic aneurysm with placement of bilateral iliac branch endoprostheses (Gore Medical, Flagstaff AZ) for his bilateral common iliac artery aneurysms via percutaneous bilateral common femoral artery access (Figures 3-6). The patient tolerated the procedure well and was discharged on post-operative day two.
Discussion
When the GORE IBE received FDA approval for treatment of common iliac artery aneurysms, it was not used bilaterally in any of the 63 patients in the pivotal study. In spite of this, there are several reports that demonstrate procedural success and favorable outcomes when used to treat bilateral common iliac aneurysm. Despite the fact that sacrifice of internal iliac arteries has been shown to be associated with a high incidence of disabling morbidity, many physicians are hesitant to utilize bilateral IBE due to the increased procedural complexity. The incidence of gluteal claudication and erectile dysfunction has been shown to approach and occasionally exceed 50 percent with internal iliac artery occlusion. The shorter recovery time, coupled with the less invasive nature of endovascular repair, make the potential morbidity of pelvic ischemia unacceptable for many patients and physicians. Furthermore, while colonic and spinal cord ischemia is infrequently reported, the effects are potentially catastrophic, and their incidence increases for bilateral internal artery sacrifice. Bilateral IBE utilization decreases the morbidity of pelvic ischemia, while maintaining the minimally invasive benefits of endovascular abdominal and iliac aneurysm repair. Furthermore, one study demonstrates only minimally increased fluoroscopy time and intravenous contrast utilization.
Conclusion
Iliac Branch Devices have increased the utility of EVAR in hostile iliac anatomy as well as transformed the treatment paradigm of iliac artery aneurysmal disease. Given the potential for significant morbidity associated with internal iliac artery occlusion, such as gluteal claudication, erectile dysfunction, colonic ischemia, and spinal cord ischemia, a strong consideration should be given to preservation of the internal iliac arteries using iliac branch devices when anatomically feasible.

Figure 1: Infrarenal abdominal aortic aneurysm

Figure 2: Bilateral common iliac artery aneurysms
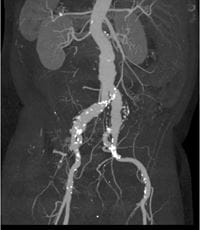
Figure 3: CTA MIP of infrarenal AAA and bilateral common iliac aneurysms
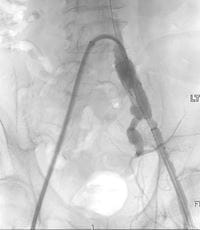
Figure 4: Positioning of the left iliac branch endoprosthesis with cannulation of the internal iliac limb

Figure 5: Positioning of the right iliac branch endoprosthesis. The up-and-over wire and the main body wire are free of wire wrap. The left iliac branch endoprosthesis is fully deployed.

Figure 6: Preparation for deployment of GORE Excluder for abdominal aortic aneurysm. Both iliac branch endoprostheses are fully deployed.
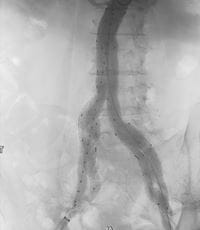
Figure 7: Completion angiogram demonstrating successful exclusion of the abdominal aortic and bilateral iliac aneurysms. Both internal iliac artery stent grafts are patent.
Bibliography
1. Greenberg RK, West K, Pfaff K, et al. Beyond the
aortic bifurcation: branched endovascular grafts
for thoracoabdominal and aortoiliac aneurysms.
.J. Vasc. Surg.; 2006;43:879–886; discussion
886-887.
2. Criado FJ, Wilson EP, Velazquez OC, et al. Safety
of coil embolization of the internal iliac artery in
endovascular grafting of abdominal aortic
aneurysms. .J. Vasc. Surg.; 2000;32:684–688.
3. Mehta M, Veith FJ, Ohki T, et al. Unilateral and
bilateral hypogastric artery interruption during
aortoiliac aneurysm repair in 154 patients: a
relatively innocuous procedure. .J. Vasc. Surg.;
2001;33:S27-32.
4. Kouvelos GN, Katsargyris A, Antoniou GA, et al.
Outcome after Interruption or Preservation of
Internal Iliac Artery Flow During Endovascular
Repair of Abdominal Aorto-iliac Aneurysms. .Eur J
Vasc Endovasc Surg.; 2016;52:621–634.